T.shivani
MBBS 9th semester
Roll no:06
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome .
I’ve been given this case to solve in an attempt to understand the topic of “patient
clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis .
Following is the view of my case..
70 yr old female with fever and left sided chest pain .January 11, 2022
A 70 year old female came to casuality on 05-01-2022 with
Cheif complaints:-
*fever since 1 day.
*Left sided chest pain since yesterday night and vomiting since 5th Jan morning 1 episode at 4 am.
History of presenting illness:-
She was apparently asymptomatic 5 days back and then she developed
- Fever, lowgrade, continuos relieved on taking medication - not associated with chills and rigors
- Left sided chest pain - radiating, pricking type of sensation to the left hand, associated with sweating, heaviness to the chest and chest tightness present.
- Vomitings in the morning at 4am - non projectile, non bilious, contains food particles and non foul smelling.
PAST HISTORY:
- Patient is a known case of diabetes and hypertension since 20 years.
- Patient is using vildaglitin(50 mg) and metmorfin(500mg) and telma(40 mg). Patient is regular with medication.
- 2007, patient had similar complains, and had a PTCA with stent implantation. She was diagnosed with triple vessel disease.
- 2015, RCA CABG done, when patient had a repeat of similar complaints.
- 2017, patient again had similar complaints, was admitted in NIMS, and conservatively treated.
- Patient has no history of thyroid, Tuberculosis or asthma.
FAMILY HISTORY:
Not significant.
PERSONAL HISTORY:
- Diet: Mixed
- Appetite: Normal
- Bowel and Bladder: Regular
- Sleep: Adequate
- No Allergies.
- Occasional Alcohol intake.
GENERAL EXAMINATION:
Patient is conscious, coherent and cooperative. Well oriented to time and space. Moderately built and moderately nourished.
After taking informed consent and in a well lit room, examination was conducted.
No pallor, icterus, clubbing, cyanosis, generalized lymphadenopathy, or edema.
Vitals:
PR- 84 bpm
BP- 130/80 mmHg measured in the left upper limb in the supine position
RR- 15 cpm
Temp- Afebrile
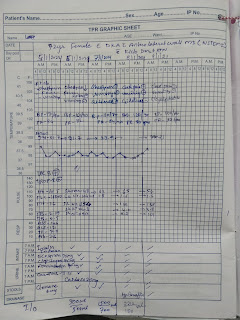
Fever chart:
Day 2: 6th jan
S: nausea,generalised weakness
No fever spikes
Pt complaining of chills
Bp :140/90mmhg
PR: 90bpm
RR : 18
Spo2 : 99% at room air
Pt is on insulin infusion since yesterday,
She had 2 episodes of hypoglycemia
Anion gap reduced (31.7 to 21)
Still continuing infusion at 2ml/hr
Day 3 : 7th Jan
S: nausea reduced ,generalised weakness
One fever spike @6pm
Temp 100.6 F
Bp :140/80mmhg
PR: 82bpm
RR : 18
Spo2 : 99% at room air
insulin infusion stopped,
No episodes of hypoglycemia
Input/ output: 1100/1000 ml
SYSTEMIC EXAMINATION:
1) Inspection:
Chest wall is symmetrical
No dilated veins, scars and sinuses.
No visible apical pulse
No visible pulsations
Visible scar is present on the midline.
2) Palpation:
Apical Pulse: Normal in the 5th intercoastal space, 1cm lateral to the midclavicular line.
No palpable pulsations
3) Percussion
Heart Borders can be percussed normally.
4) Auscultation:
S1, S2 sounds are heard.
No abnormal heart sounds heard
1) Inspection:
- Chest is symmetrical
- Trachea is in the midline
- No drooping of shoulders
- No sinuses and dilated veins
2) Palpation:
- Trachea – midline
- No dilated veins
- Chest movement is symmetrical
3) Percussion:
R L
Infraclavicular Resonant Resonant
Mammary. Resonant Resonant
Axillary. Resonant Resonant
Infraaxillary Resonant Resonant
Suprascapular Resonant Resonant
Infrascapular Resonant Resonant
4) Auscultation:
-Breath sounds: Normal Vesicular Breath sounds
- No added breath sounds
1) Inspection:
- Shape: scaphoid, not distended
- Flanks: free
- Umbilicus: midline, inverted
- Skin: not stretched, shiny, no scars, sinuses, striae
- No dilated veins
- No abnormal movements of the abdominal wall, visible peristalsis,
2) Palpation:
- No local rise in temperature, no tenderness
- Soft on touch
3) Percussion:
- No fluid thrill, shifting dullness
4) Auscultation:
- Normal bowel sounds heard
- Normal higher mental functions
- No focal neurological deficit
- All higher motor functions are normal
Investigations:
TROP - 1 is positive.
ECG:-
05-01-2021
06-01-2021
2D echo :
DIAGNOSIS:
DKA with anteroinferior wall MI
TREATMENT:
1. Inj. HAI 1 ml (40 U) + 39 ml NS at 8 ml/hr to maintain GRBS less than 200 mg/dl
2. IVF. 1 unit NS continuous infusion at urine output + 30ml/hr
3. TAB ECOSPORIN 75 MG PO OD
4. TAB CLOPIDOGREL 75 MG PO OD
5. TAB CARDIVAS 3.125 MG PO BD
6. INJ. CLEXANE 60 MG S/C BD FOR 5 DAYS
7. TAB MONIT GTN 2.6 MG PO OD
8.TAB ATORVASTATIN 40 MG PO BD



















Comments
Post a Comment